UMass Medical School scientist Gang Han, PhD, and his team have designed a new class of molecules used in photodynamic therapy that are able to direct lamp light deep into tissue to kill cancer tumors and possibly provide greater accessibility at a lower cost to patients. This work is supported by the Human Frontier Science Program and NIH.
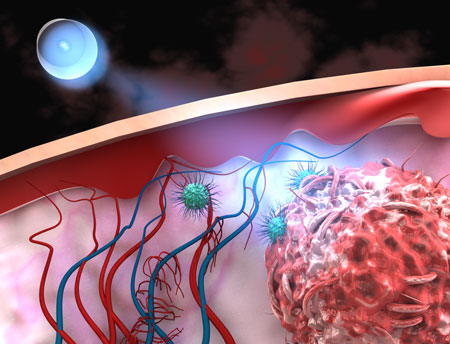
Figure: Ultra-low power lamp light to kill cancer tumors photodynamically in deep tissue with highly NIR-sensitive organic nanoparticles
In a recent paper published in the Journal of the American Chemical Society, Dr. Han, Associate Professor of Biochemistry and Molecular Pharmacology, outlines how the carbazole-substituted BODIPY (Car-BDP) molecules, which possess an intense, broad NIR absorption band with a remarkably high singlet oxygen quantum yield, will further the potential clinical application for photodynamic therapy (PDT).
“This study signals a major step forward in photodynamic therapy by developing a new class of NIR-absorbing biodegradable organic nanoparticles for highly effective targeting and treatment of deep-tissue tumors,” Han said.
Tissue penetration depth is a major challenge in practical photodynamic therapy (PDT). Traditionally, PDT involves the patient receiving a non-toxic light-sensitive drug, which is absorbed by all the body’s cells, including cancerous ones. A red laser light specifically tuned to the drug molecules is then selectively turned on in the tumor area. When the red light interacts with the photosensitive drug, it produces a highly reactive form of oxygen (singlet oxygen) that kills the malignant cancer cells while leaving most neighboring cells unharmed.
Based on research by the Han Lab at UMMS and colleagues, the process might become simpler, more effective and cost efficient.
Han explains that after being encapsulated with biodegradable polymers, Car-BDP molecules can form uniform and small organic nanoparticles that are water-soluble and tumor targetable. Used in conjunction with a record low-power-density and cost-effective incoherent lamp light rather than the coherent high power laser light that has to be used in the existing PDT therapy, the molecules can be tracked as they spread through the body deep into the tissue to outline and kill cancerous tumors. More interestingly, these organic nanoparticles were found to have an extremely long circulating time before being removed from the body, which is essential for the new PDT drug development.
Han said the combination is “sufficient to monitor and trigger PDT effect of these nanoparticles within a wide variety of deep-tissue level tumors such as lung, colon, prostate and breast cancers.”
In addition, the potential new platform for precise tumor-targeting theranostics and novel opportunities with low power lamp light could allow for future affordable clinical cancer treatment that patients may be able to manage in their homes or to resource deficient areas, such as on battlefields and in developing countries.
Reference
Ultralow-Power Near Infrared Lamp Light Operable Targeted Organic Nanoparticle Photodynamic Therapy. Huang L, Li Z, Zhao Y, Zhang Y, Wu S, Zhao J, Han G. J. Am. Chem. Soc., 2016, 138 (44), pp 14586–14591. DOI: 10.1021/jacs.6b05390.


































